

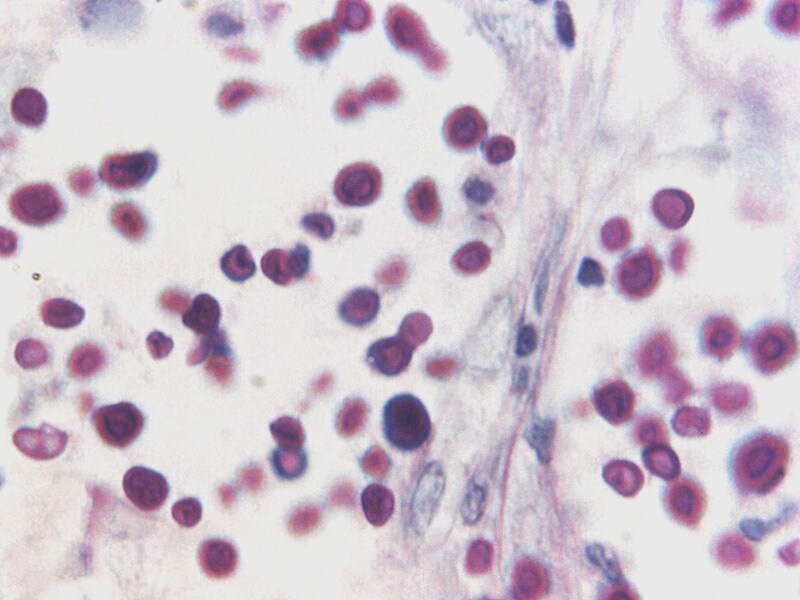
Some previous studies have suggested that low baseline CSF white cell count (WCC) was a predictor for poor clinical outcomes in CM patients, but other studies showed that CSF WCC was not associated with clinical outcomes. More importantly, dynamic changes in CSF cell count could help assess disease status and therapeutic response. CSF cytology and cell count can provide quick and cost-effective important information on possible etiologies that could lead to diagnosis and guide immediate therapeutic decisions. However, several CrAg measurements are probably unhelpful for CM management because CrAg can still be positive even if the pathogen has been cleared. Many previous studies have shown that high CSF CrAg titer (>1:1024) was an independent risk factor for poor prognosis in CM patients. CSF cellular analysis, India ink staining, CSF Cryptococcal antigen (CrAg) test, fungal culture, and molecular techniques are used to diagnose CM. Accurate analysis of the cerebrospinal fluid (CSF) profile is essential when diagnosing and managing CM. Aggressive management of elevated intracranial pressure via LP is beneficial to CM patients. Lumbar puncture (LP) is a common procedure in CM patients. Recent advances in the care for CM patients and CM prevention, including some new agents and adjunctive immunomodulatory therapies, have the potential to reduce mortality from the disease. However, in recent years, CM has been on the rise in HIV-negative hosts with organ transplants, autoimmune disease, immune deficiencies, hematological malignancies, prolonged immunosuppressants treatment, and even in apparently immunocompetent individuals. The incidence of CM in HIV-infected patients has decreased in the era of antiretroviral therapy. Moreover, 15% (95% CI, 10–19%) of Acquired Immune Deficiency Syndrome (AIDS) patients died from CM. Globally, an updated data from 2017 show that annual deaths from CM are about 181,100. It is an opportunistic fungal infection common among human immunodeficiency virus (HIV)-infected patients, particularly in sub-Saharan Africa. , is responsible for significant morbidity and mortality and requires prolonged treatment. Our results indicated that baseline CSF WCC and changes in CSF WCC over time could be used to assess the prognosis of CM patients.Ĭryptococcal meningitis (CM), caused by Cryptococcus spp. The predictive model incorporating longitudinal data of CSF WCC had better sensitivity, specificity, and accuracy than a model incorporating only baseline CSF WCC data. The best cut-off value to predict a poor clinical outcome was 40 cells/μL during baseline CSF WCC. Baseline CSF WCC had a moderate positive correlation with peripheral CD4+ T lymphocyte count ( r = 0.738, P < 0.001) and CD4+ T lymphocyte percentage ( r = 0.616, P < 0.001). CM patients with triple therapy during the induction period presented with a better clinical outcome ( P<0.05). ResultsĬM patients with lower baseline CSF WCC, CSF protein concentration or CD4/CD8 ratio, and those with altered mentation or HIV coinfection were more likely to have poor clinical outcome ( P<0.05). We retrospectively analyzed the medical records of 150 CM patients admitted to our hospital between January 2008 and December 2018. Using longitudinal data of CSF WCC and its relationship with clinical outcomes in CM patients, we aimed to elucidate the clinical significance of this test. However, the clinical significance of CSF white cell count (WCC) in CM patients is not fully understood. Cerebrospinal fluid (CSF) cytology and cell count are very important for CM on etiology diagnosis and assessment of disease status and therapeutic response. The incidence of cryptococcal meningitis (CM) has gradually increased in recent years.


 0 kommentar(er)
0 kommentar(er)
